Gene therapy in cancer treatment: how nanomaterials solve delivery issues
Written by Dr. Anna Bogdanska
According to the World Health Organisation (WHO), cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020. In Ireland, 1 in 4 deaths is caused by cancer. Cancer occurs when there is a disruption to the cell growth and function caused by damage (mutation) to genes within those cells. Gene therapy is an emerging form of treatment where genetic material is delivered to defective cells to either insert a missing gene, correct, or delete a mutated gene or to deliver a therapeutic gene. Despite the immense potential of this type of therapy, there are many obstacles preventing novel gene therapy formulations from advancing into clinic.
Delivering genetic material to cells of interest is one of the biggest challenges in developing a successful gene therapy. Genetic material injected directly into the bloodstream would be exposed to a number of enzymes which could degrade it before reaching target cells. Furthermore, genetic material cannot be easily inserted into a cell and requires a form of carrier called a vector. Think of it as a Trojan horse used to protect the cargo material from enzymes present in the blood and “trick” cells into taking up foreign genetic material. An ideal vector should be able to accommodate foreign genes of sufficient size, not trigger an immune response, and deliver gene to a specific cells.
Deactivated (“turned off”) viruses are commonly used as vectors in gene therapies. In this type of formulation, a viruses’ natural ability to infect cells is hijacked to deliver therapeutic genes. Unfortunately, viral vectors suffers from bad reputation as term virus is often associated with disease and mortality. Indeed, side effects of this vector can include an immune response, and for this reason research in the area of gene therapy has recently shifted towards the use of nanomaterial based delivery systems.
Nanomaterials are defined as materials with one or more external dimensions in the size range between 1 and 100 nanometres. For the past few decades there has been a rapid rise in the use of nanomaterials in a wide range of biomedical applications, with extensive research now focused on using this technology in gene therapy. We have witnessed effectiveness of nanomaterial based vectors during the global coronavirus disease 2019 (COVID-19) pandemic. Two vaccines (Spikevax® and Comirnaty®) used a type of nanomaterial called a liposome to deliver a single stranded genetic material, messenger RNA (mRNA) which codes for the production of antibodies against the spike protein on the coronavirus. Unlike some of the viral vectors, nanomaterial based delivery systems are considered biocompatible with a low risk of causing an immune response. Additionally, they can accommodate larger genes in comparison to viral vectors and can be relatively easily modified to target specific cells making them superior over traditional viral vectors. Figure 1 highlights some of the benefits of using nanomaterial based vectors in comparison to traditional viral vectors.
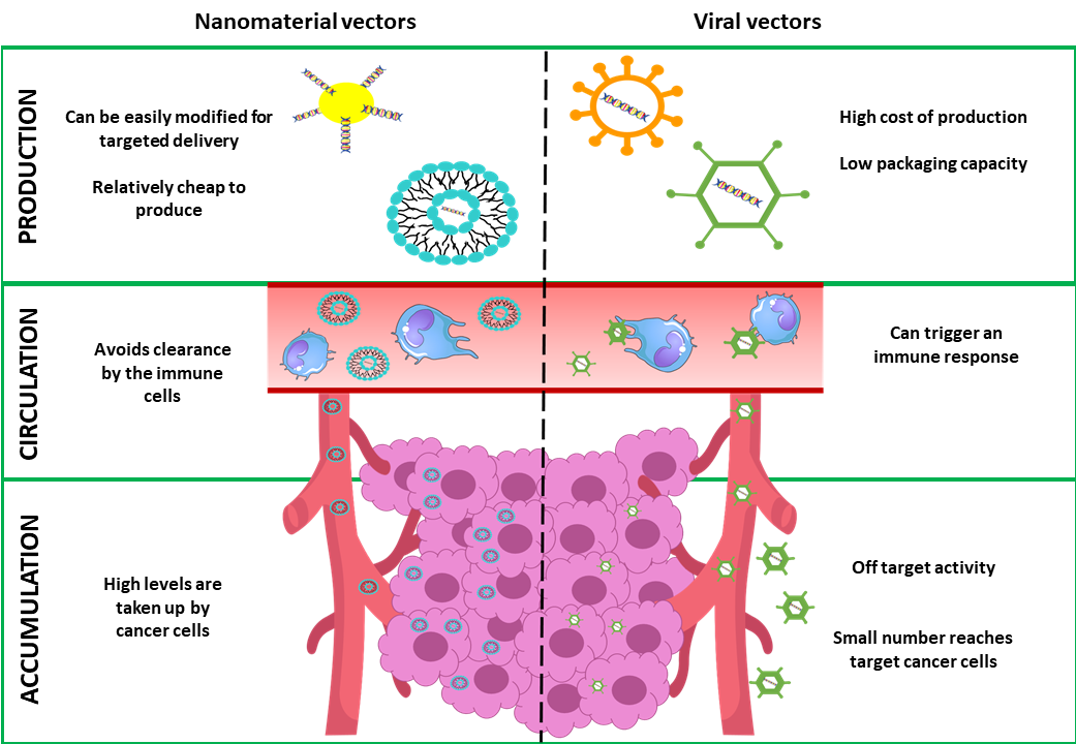
Figure 1: Comparison between nanomaterial based vectors and viral vectors for cancer gene therapy
Graphical representation of how nanomaterial based vectors (left hand side) overcome limitations of traditional viral vectors (right hand side) in cancer gene therapy. Image not to scale.
Our POI project led by Professor Tracy Robson, aims to harness the potential of nanomaterials in gene therapy for ovarian cancer. Over the past few years we have been investigating a protein called FK506-binding protein like (FKBPL). Our results indicate that this protein plays a role in inhibiting a number of processes occurring in cancer such as formation of new blood vessels (angiogenesis), tumour growth, and cancer cell migration, with the end result of slowing tumour growth. In order to increase the amount of FKBPL produced by ovarian cancer cells, we will deliver an artificial gene (transgene) coding for this protein using a peptide based nano-delivery system called RALA. This new technology allows us to deliver full FKBPL gene, something we could not achieve before. Although our research is still in its infancy, nanoparticle vectors have already solved one of the big delivery issues. We are excited to further investigate how this novel gene therapy will perform in treating ovarian cancer, with hope of bringing it to clinical trial.
Author: Dr. Anna Bogdanska
.jpg)
Author’s note:
After completing my undergraduate degree in Biomolecular sciences in Technological University Dublin, I interned at the department of Obstetrics and Gynaecology in Trinity College Dublin. I have recently completed my PhD in the Nanomedicine and Molecular imaging group in Trinity College Dublin, during which I had an opportunity to contribute to a number of pre-clinical studies of novel nanomaterials for medical applications. I am excited to work as a Postdoctoral Researcher on this project, under the supervision of Professor Tracy Robson. I hope that my personal interest and experience in areas of ovarian cancer and nanomedicine research will benefit the project with an ultimate goal of delivering a new personalised treatment to ovarian cancer patients.