Blood Cancer Biobank Ireland - supporting translational and clinical research
Written by Tatiana Cichocka
Blood cancers such as acute myeloid leukaemia (AML), multiple myeloma (MM), and chronic lymphoid leukaemia (CLL) are very rare and complex diseases. They are very variable, or heterogenous, at the genetic, cellular, and microenvironment levels, making both the treatment development and decisions on treatment very difficult. Although some advances have been made over the last decades in treatment for some of these cancers, many still remain difficult to treat.
Biobanks are a crucial part of research. This article sums up the role of biobanks in cancer research in Ireland.
In order to come up with better treatment for blood cancers, a lot of translational and clinical research is required. This involves screening the proposed treatment on a large set of patient samples to find out whether it is widely effective. Typically, the number of patient samples one can obtain is the bottleneck to these studies, as blood cancers are rare.
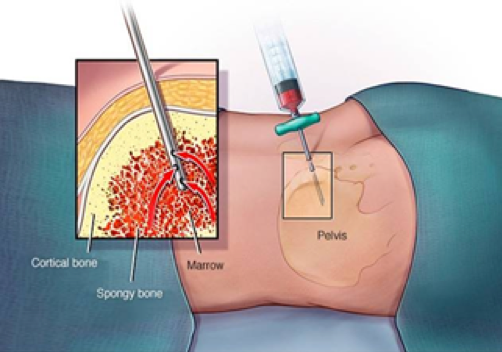
Blood Cancer Network Ireland (BCNI) alleviated that problem for haematology researchers in Ireland by setting up a national blood cancer biobank. A biobank is a collection of biospecimens, such as biopsies from tissues. In the case of the blood cancer biobank, it is a collection of bone marrow and blood samples from blood cancer patients. For storage, the samples need to be processed, which has to be done by highly trained staff using standard operating procedures (SOPs). Moreover, throughout the sample processing, many quality control steps are taken to ensure the highest sample quality. All procedures are well documented and fully GDPR compliant.

I am the manager of the Blood Cancer Biobank and my job is to manage (and partially carry out) the process starting with the collection of the samples at the hospitals to its storage and its final usage in research projects. My work starts when I get a call from the hospital that a patient suspected of having blood cancer has offered to donate a sample to the biobank. If the patient consents, a sample of bone marrow and/or peripheral blood is taken for the biobank alongside their clinical diagnostic sample. Samples can also be collected after the completion of treatment and upon relapse from the same patient. I either pick up the sample myself, if it's from our local hospital, or if it was collected in a hospital in another city, the hospital staff couriers the sample to the biobank lab. I will then process the arrived samples in the biobank laboratory, by separating the samples into a range of fractions. These include the blood plasma, mononuclear cells (most white blood cells that include the cancerous cells), and bone marrow stromal cells. These are then stored in ultra-low temperatures until needed by researchers.
The stored samples are highly annotated on the biobank’s database. The annotation includes the patient’s clinical data (precise diagnosis, treatment details, and the response to the treatment) and biospecimen data (cell concentration, number of tubes frozen down, and the precise location of the sample). It is also my job to be sure that all sample tubes (which are labeled with individual QR codes) have their storage location recorded in the biobank’s data management system, and this is annotated with the patient’s clinical information.

The samples we store can support both translational and clinical research either through prospective sample collection or through the use of already collected samples. Any researcher with an ethically approved study can apply for the use of biobank samples. When studies get approved for use of biobanked samples, it is my job to retrieve the samples from storage and provide them to the research team.
Currently over 500 patient samples are stored within the Blood Cancer Biobank, equalling about 15,000 tubes. This was collected by 7 different hospitals across Ireland, which are part of BCNI. As a result, even if a researcher is looking for a specific subtype of blood cancer or patients that received a certain kind of treatment, there should be a choice of samples for that study.

One study that biobanked samples were used for was to determine if an in-vitro assay could be set up to determine a patient’s response to the standard-of-care chemotherapy used to treat AML. 36 AML patient samples were tested (which were previously biobanked), and the clinical response of the patient was obtained from the treating hospitals. It was found that by keeping the AML cells together with the stromal cells of the bone marrow, it was possible to predict the patient’s response to the drug treatment within days as opposed to weeks in the clinic. This could be clinically relevant, as the results may allow clinicians to change the treatment approach if they know that the patient will not respond to the treatment.
Another study the biobank is currently involved in looks at the response of chronic lymphocytic leukaemia (CLL) patients to COVID vaccines. CLL patients, due to impaired B cell production, are immunocompromised and they are known to have an incomplete response to immunization. The study aims to understand better the actual efficacy of COVID vaccination in these patients, and whether booster vaccines can improve it.
A blood cancer biobank is an invaluable tool for the haematology community in Ireland. It can provide a solution to conducting more thorough studies in a shorter timeframe than otherwise would be possible, leading to improved treatment options for future blood cancer patients.
Author: TATIANA CICHOCKA

Tatiana is the manager of the Blood Cancer Biobank Ireland, a national effort focused on coordinating and standardising blood cancer biobanking activities at sites in Galway, Dublin, Cork, Limerick and Waterford. The biobank is co-ordinated by the Blood Cancer Network Ireland, led by POI Investigator Dr. Eva Szegezdi, and based in the National University of Ireland, Galway.

